By Rachel McDonald, the Australian Science Media Centre
A cancer therapy that is already being used to effectively cure some patients with aggressive blood cancers could one day be used to fight a host of other cancers, according to Australian researchers. The team have combined the therapy, known as CAR T-cell therapy, with gene-editing technology to test its ability to fight solid cancers in mice.
Speaking at an AusSMC media briefing, Co-Head of the Cancer Immunology Program at the Peter MacCallum Cancer Centre Phil Darcy explained that CAR T Cell therapy is a "specialised form of immunotherapy using a patient's own T-cells to fight their cancer."
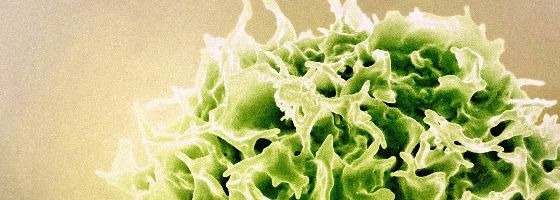
T-cells are a type of white blood cell that are central to the body's immune system.
Professor Darcy said the process involved collecting a patient's T-cells and modifying them with a chimeric antigen receptor, or CAR, to bind to proteins found in abundance on cancer cells, which essentially trains the T-cells to recognise and kill cancer cells once reintroduced into the body.
"Remarkably, these CAR T-cells have been shown to cure aggressive blood cancers where all other treatments have failed," Prof Darcy said.
However, he said scientists have so far been unable to replicate the impressive results when it comes to solid cancer tumours, with the T-cells struggling to survive in great enough numbers to find and penetrate the tumour.
Associate Professor Paul Beavis, also Co-Head of Peter Mac's Cancer Immunology Program, said researchers have been trying to address this by engineering the T-cells to express an 'armour' gene that makes it easier to find the cancer. This gene causes inflammation, which can attack the tumour, however, if this inflammation occurs elsewhere in the body, the patient can become too sick.
A/Prof Beavis said their team's potential solution to this new problem is to use a gene editing tool called CRISPR, which allows them to rewire the 'armour' gene to only be released at the site of the tumour rather than throughout the body.
The researchers tested this technique by modifying mouse T-cells, and testing them on mice with solid tumours. A/Prof Beavis said they saw "drastic" responses at the tumour site, without the T-cells harming the mice in other areas of the body.
"In our study, we checked all of the major organs such as the blood, liver, brain, kidneys and lungs, and we saw no expression of our armouring gene, and we saw it only in the tumour site," he said.
He said the team also saw positive results when testing human T-cells against human tumours in mice, which was an important step toward full human trials.
This technology can be used on any type of CAR T-cell, which the researchers say means it could be used to tackle a range of different cancer types, with five human CAR systems already tested in their study.
Prof Darcy said the broad potential of the technology was one of its benefits, with cancers that currently have low survival rates, such as pancreatic and ovarian cancer, among the potential targets of the treatment.
"As long as we have a good target for the CAR T-cell, we can apply the technology to those really difficult to treat cancers, such as pancreatic cancer," he said.
Prof Darcy said the technology also appeared to work whether the T-cells are derived from the patient or a healthy donor.
He said donor-origin T-cells are currently a focus in other research as a potential lower-cost, "off-the-shelf" option where health professionals can take T-cells from an existing donor collection rather than extracting them from an individual patient, although patients' bodies are more likely to reject the treatment using this approach.
A/Prof Beavis said the team were currently exploring funding to begin human trials, likely with multiple myeloma or solid tumour patients. Once funding is secured, he said trials could be underway within the next five years.
You can read more about the briefing here
This article originally appeared in Science Deadline, a weekly newsletter from the AusSMC. You are free to republish this story, in full, with appropriate credit.
Contact: Rachel McDonald
Phone: +61 8 7120 8666
Email: info@smc.org.au